For more information about current studies please email Hypoglycemiastudy@joslin.harvard.edu or call (617) 309-1940
Please let us know where you live, and if we may contact you regarding future in-person or potential remote studies.
Studies of New Treatment Approaches for Hypoglycemia
Lucidity Study to Evaluate Avexitide, a Medication which Blocks Action of the Hormone GLP1 - ongoing
Pasiphy Study to Evaluate Pasireotide as a New Treatment for Post-Bariatric Hypoglycemia - ongoing, recruitment closed
Developing a Glucagon Pump to Treat Post-Bariatric Hypoglycemia - ongoing studies of how glucagon works, the dose needed, and ultimately how to deliver glucagon via a pump for treatment. This is an ongoing study for which we are recruiting!
Understanding the Causes of Post-Bariatric Hypoglycemia and Identifying New Approaches to Treatment of this Condition - These studies often involve procedures to help us understand contributors to hypoglycemia and may/may not involve research medications. Below are some examples of how these studies tell us more about hypoglycemia. You may also wish to look at the Hypoglycemia Clinic page of this website.
Congrats to our team on the publication of our paper in Nature Metabolism (2025)! In this paper we identify alterations in bile acid signaling in patients with post-bariatric hypoglycemia. We thank the entire research team and our volunteers who give so generously of their time and blood and stool samples to find new approaches to treat hypoglycemia! We are hoping to begin translating these findings soon. See PDF below.
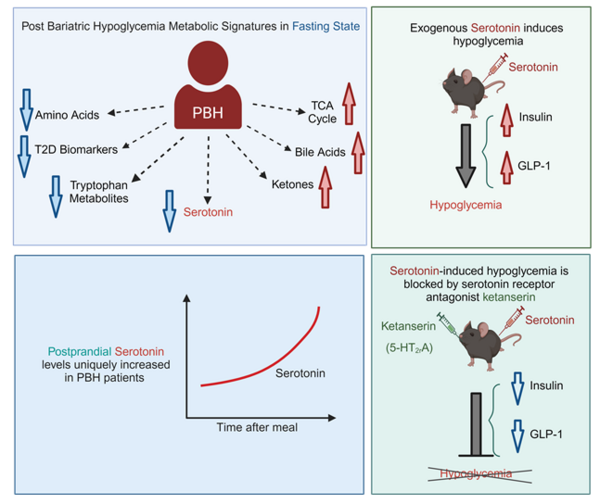
Congrats to postdoctoral fellow Rafael Ferraz-Bannitz and the entire team on the publication of our paper in Journal of Clinical Investigation (2024)! We identify alterations in serotonin-dependent signaling as a potential contribution to post-bariatric hypoglycemia. We thank the entire research team and our volunteers who give so generously of their time and blood samples to find new approaches to treat hypoglycemia! We are hoping to begin translating these findings, but are awaiting decisions regarding research funding! The PDF is posted below.
Determining the Efficacy of Continuous Glucose Monitoring to Reduce Hypoglycemia and Improve Safety in Patients with Hypoglycemia after Gastric Surgery
*This study has been completed! Results were presented at the 2023 American Diabetes Association and published in the medical journal Diabetes Obesity and Metabolism:
Continuous glucose monitoring in patients with post-bariatric hypoglycaemia reduces hypoglycaemia and glycaemic variability. Cummings C, Jiang A, Sheehan A, Ferraz-Bannitz R, Puleio A, Simonson DC, Dreyfuss JM, Patti ME.Diabetes Obes Metab. 2023 Aug;25(8):2191-2202. doi: 10.1111/dom.15096. Epub 2023 May 3.PMID: 37046360
The conclusions of this study: Real-time CGM data and alarms are associated with reductions in low sensor glucose, elevated sensor glucose, and glycaemic variability. This suggests CGM allows patients to detect hyperglycaemic peaks and imminent hypoglycaemia, allowing dietary modification and self-treatment to reduce hypoglycaemia. The use of CGM devices may improve safety in PBH, particularly for patients with hypoglycaemia unawareness.
Mechanisms of Post-Bariatric Hypoglycemia:
Enrollment has been completed, and analysis of data is in progress. A small part of the results has been published (JCI, 2024, Nature Metabolism, 2025, Clinical Endocrinology 2024). See below for the PDFs.
Mechanisms of Hypoglycemia in Patients without Diabetes:
Analysis of data is in progress.
Hypoglycemia and the Gut Microbiome: Analysis of the data from this study is in progress. Some of the results were included in the bile acid manuscript (Nature Metabolism, 2025). See PDF below.
Understanding the Role of Bariatric Surgery as a Treatment for Type 2 Diabetes
The ARMMS-T2D Study
- The first report from this study was just published in JAMA (Journal of American Medical Association) in February 2024! Additional data analysis is in progress, so stay posted!
- Long-Term Outcomes of Medical Management vs Bariatric Surgery in Type 2 Diabetes. Courcoulas AP, Patti ME, Hu B, Arterburn DE, Simonson DC, Gourash WF, Jakicic JM, Vernon AH, Beck GJ, Schauer PR, Kashyap SR, Aminian A, Cummings DE, Kirwan JP.JAMA. 2024 Feb 27;331(8):654-664. doi: 10.1001/jama.2024.0318.PMID: 38411644
-
Abstract of manuscript:
-
Importance: Randomized clinical trials of bariatric surgery have been limited in size, type of surgical procedure, and follow-up duration. Objective: To determine long-term glycemic control and safety of bariatric surgery compared with medical/lifestyle management of type 2 diabetes. Design, setting, and participants: ARMMS-T2D (Alliance of Randomized Trials of Medicine vs Metabolic Surgery in Type 2 Diabetes) is a pooled analysis from 4 US single-center randomized trials conducted between May 2007 and August 2013, with observational follow-up through July 2022. Intervention: Participants were originally randomized to undergo either medical/lifestyle management or 1 of the following 3 bariatric surgical procedures: Roux-en-Y gastric bypass, sleeve gastrectomy, or adjustable gastric banding. Main outcome and measures: The primary outcome was change in hemoglobin A1c (HbA1c) from baseline to 7 years for all participants. Data are reported for up to 12 years. Results: A total of 262 of 305 eligible participants (86%) enrolled in long-term follow-up for this pooled analysis. The mean (SD) age of participants was 49.9 (8.3) years, mean (SD) body mass index was 36.4 (3.5), 68.3% were women, 31% were Black, and 67.2% were White. During follow-up, 25% of participants randomized to undergo medical/lifestyle management underwent bariatric surgery. The median follow-up was 11 years. At 7 years, HbA1c decreased by 0.2% (95% CI, -0.5% to 0.2%), from a baseline of 8.2%, in the medical/lifestyle group and by 1.6% (95% CI, -1.8% to -1.3%), from a baseline of 8.7%, in the bariatric surgery group. The between-group difference was -1.4% (95% CI, -1.8% to -1.0%; P < .001) at 7 years and -1.1% (95% CI, -1.7% to -0.5%; P = .002) at 12 years. Fewer antidiabetes medications were used in the bariatric surgery group. Diabetes remission was greater after bariatric surgery (6.2% in the medical/lifestyle group vs 18.2% in the bariatric surgery group; P = .02) at 7 years and at 12 years (0.0% in the medical/lifestyle group vs 12.7% in the bariatric surgery group; P < .001). There were 4 deaths (2.2%), 2 in each group, and no differences in major cardiovascular adverse events. Anemia, fractures, and gastrointestinal adverse events were more common after bariatric surgery. Conclusion and relevance: After 7 to 12 years of follow-up, individuals originally randomized to undergo bariatric surgery compared with medical/lifestyle intervention had superior glycemic control with less diabetes medication use and higher rates of diabetes remission.
Understanding How Metabolism and Diabetes Can Affect Men's Health and Reproduction
- The JEST Study: Enrollment has been completed, and analysis of the data from this study is ongoing.
Please contact Dr Patti at mary.elizabeth.patti@joslin.harvard.edu if you are interested in learning more about any of these studies!
